Menu
Log in
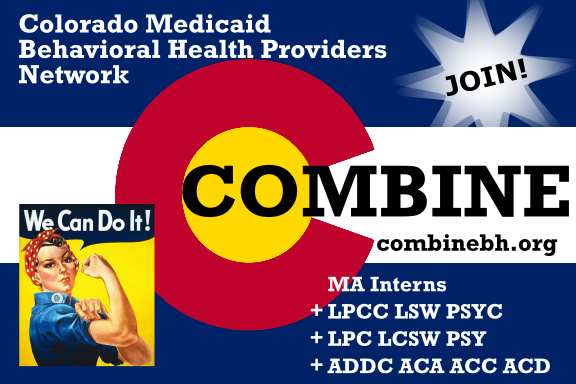
Counselors - Peers - Marriage and Family Therapists - Addiction Counselors
Psychologists - Social Workers - Pre-licensure Professionals - Interns
...for a diverse, competent, and sustainable behavioral healthcare workforce.
Donation goal
Larger clinics that see real benefits from COMBINE efforts please donate 1/10th of 1% of Medicaid revenue. (e.g. $500 on $500,000)
101%
Collected: $18,149.00
Goal: $18,000.00
|
Powered by Wild Apricot Membership Software


.png)